REBECCA DALZELL
Bec Dalzell is the Haemophilia Physiotherapist at the Royal Brisbane & Women’s Hospital
No one wants to be called ‘old’! Most of us feel young at heart and hate to consider that our bodies are experiencing anything different! Unfortunately once we pass early adulthood we are all in a gradual state of decline. Even before we feel it, we are beginning to wear out. Our joints deteriorate, our muscles don’t work as well as they used to, our balance declines and our bones become less dense. These are unavoidable facts! For many, this decline slips by unnoticed for many years, until it suddenly starts to become apparent in later life. For others, including those with bleeding disorders, the starting point is often compromised, and the signs of this process can begin to present themselves earlier…Let me explain.
People with bleeding disorders have been shown to have poorer balance when compared to others of the same age, and this begins in childhood. Joint bleeds and joint damage can alter what is called proprioception (our awareness of where our body is in space) and this, among other factors, can contribute to decreased balance reactions. Many may not be aware of this deficit, or the need to address it – until it’s too late!
Bone density in those with severe bleeding disorders has also been shown to be decreased, beginning in childhood, when compared with controls. There are numerous possible contributing factors here including:
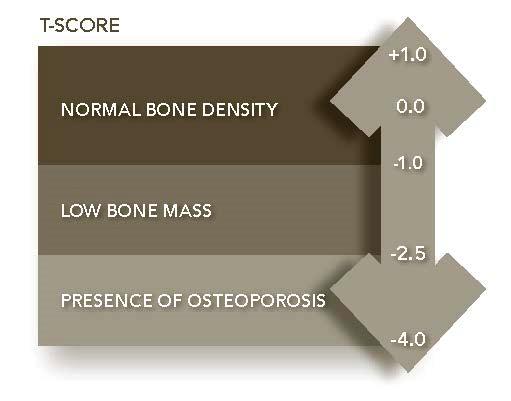
Decreased BMD may initially be asymptomatic, but ongoing decline can lead to osteoporosis and increased risk of fracture. These factors, along with haemophilia-related joint damage, pain, and decreased joint range of motion, mean that those with bleeding disorders are at increased risk of falls and fracture (even though they may not know it) – and this can have serious consequences.
Studies done in the general population show that 30% of those over 65, and 50% of those over 80 fall each year. 20-30% of those in the general population who fall suffer injuries that reduce mobility and independence and increase the risk of premature death. For those with bleeding disorders these statistics would most likely be higher due to the presence of additional falls risk factors.
It’s not all bad news. Your Haemophilia Treatment Centre Physiotherapist can help! There are a huge range of activities you can do with your Physiotherapist to help improve balance, optimise BMD, prevent falls and enhance quality of life. Many of these problems can be averted.
Physical activity has been shown to have numerous benefits. Research shows that balance can be improved, and most falls prevented, through physical activity. Exercise programs that address strength, balance, flexibility and/or endurance (2-3 of these components) have been shown to significantly reduce the rate of falls, and the number of people falling.
BMD can also be positively influenced by exercise. For those who are younger – teens to early twenties – exercise can significantly help to build strong bones to optimise peak BMD (giving you a much better starting point for the rest of your life!). For those who are more mature, it has been shown that BMD can be maintained, if not slightly improved, and bone turnover decreased, through strength training and weight bearing exercise (3). Hip fractures have been found to be nearly half as frequent in adults who have been physically active in their daily life compared to less active people.
Physical activity also helps reduce pain, improve joint nutrition, strengthen muscles, improve joint stability, preserve and possibly improve joint range of movement, assist in weight control, improve posture, and prevent secondary musculoskeletal complications. These all help to maintain function and prevent many of the associated adverse health outcomes.
There are also many health and environmental factors that can both optimise BMD, and reduce falls risk, significantly reducing the risk of fracture. These will be explained further below.
ACTION PLAN:PREVENTION IS THE BEST MEDICINE
Participate in physical activity throughout life
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine