ANDREW ATKINS
Andrew Atkins is Nurse Consultant, SA Adult Haemophilia Treatment Centre, Royal Adelaide Hospital
Muscle bleeds are the second most common sites of bleeding in haemophilia (after joint bleeding), and iliopsoas muscle bleeds are known to be a muscle at risk of bleeding. However, if you’re a person with haemophilia and you’ve never suffered an iliopsoas bleed before, chances are you’ve never heard of this muscle.
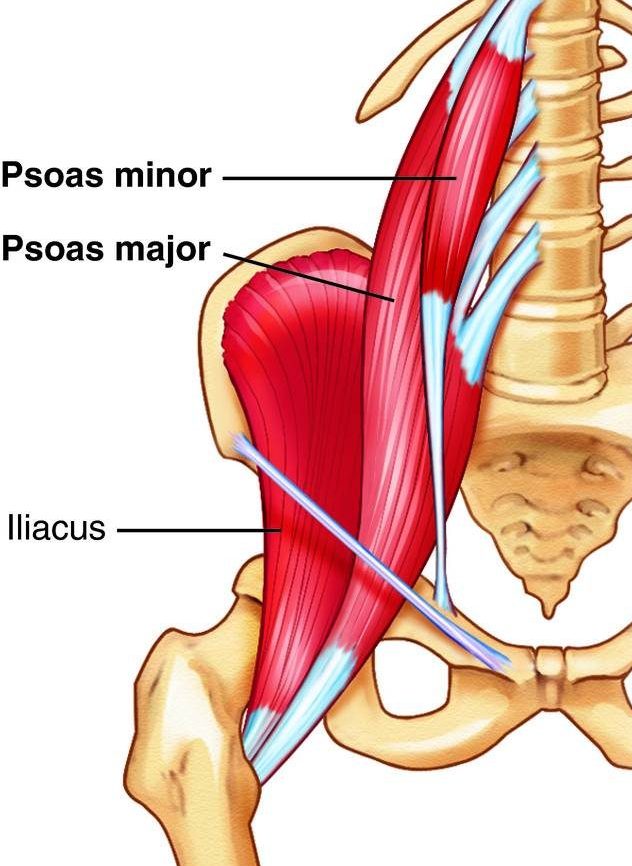
The iliopsoas muscle is made up of the iliacus and psoas muscles combined. It is a large muscle attaching to your spine, pelvis and femur. The iliopsoas muscle is the only muscle that connects the spine to the leg. The muscle allows you to bend from the hip (i.e., to walk up stairs or pick something up from the floor), to sit up, and to move the leg forward to walk or run. It stabilises the spine and helps with posture. Structurally it is the deepest muscle in the body.
A bleed into the iliopsoas muscle may not be easily recognisable if you have not had one before or don’t know what to look out for. Because the muscle is large, a lot of blood can be lost into it, which can obviously be serious – but this also means initially it may not appear serious because the pain from bleeding may not be as intense as a joint bleed feels. There are also a number of nerves in the region of this muscle, notably the femoral nerve. If this nerve is, compressed, it causes loss of sensation and may take months to resolve, with long-term or even permanent disability if the bleed is not treated in time or adequately.
You may experience some or all of these:
Iliopsoas bleeds may occur due to an injury, or in severe haemophilia can occur spontaneously without an apparent cause. A scan (either ultrasound, CT or MRI) is usually required to confirm the diagnosis.
If you suspect you have an iliopsoas bleed, and you have home treatment, then treat immediately using the treatment plan previously given to you by your Haemophilia Treatment Centre (HTC) for a muscle bleed. Whether you self-treat or not, you should attend your nearest hospital’s Emergency Department, preferably at your HTC hospital. This is especially important if you have any numbness or tingling sensation down your leg. Rest as much as possible in the meantime, and use crutches or a walking aid. Get someone to drive you rather than driving yourself.
Treatment of an iliopsoas muscle bleed will be prolonged. Factor levels will need to remain raised to a high level for an extended number of days, along with strict bed rest. Blood tests for monitoring levels may be needed. For these reasons often a hospital admission is required, so that progress can be monitored closely. A physiotherapist should be involved with your care to provide advice during the acute stage of the bleed, and then to provide ongoing instruction and an exercise regime as improvement is made. Expect progress to a full recovery to be slow.
It is important to avoid re-bleeding into the muscle – if it occurs it will be more severe and will definitely delay your return to full capacity for everyday activities. Follow the advice of your HTC team, and particularly the physiotherapist. It is also important to establish the cause for the bleed, if at all possible, and it may help to have a frank discussion with someone from your HTC team to look at ways to prevent it happening again.
REFERENCES
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine