CAT POLLARD
Cat Pollard is Advanced Clinician Physiotherapist, Auckland Regional Haemophilia Service
This article is reprinted with permission from Bloodline, the magazine of the Haemophilia Foundation of New Zealand (www.hfnz.org.nz), vol. 47 no. 3, December 2019.
The musculoskeletal care of people with bleeding disorders is highly specialised with the ultimate goal of minimising joint arthropathy. The Australia and New Zealand Physiotherapy Haemophilia Group (ANZPHG) are a core group of dedicated haemophilia physiotherapists who aim to provide best evidence care to those living with bleeding disorders. For this edition of National Haemophilia, Cat Pollard has kindly shared an article that she wrote for the Haemophilia Foundation of New Zealand (HFNZ) about the integration of ultrasound scanning into haemophilia care. Cat is the Advanced Specialist Physiotherapist for Haemophilia in the Auckland District of New Zealand and a valued member of the ANZPHG.
Alison Morris, Australian co-chair, ANZPHG

We are donning our X-ray vision goggles and looking deeper into joints than ever before. Well, not really, but at a number of Haemophilia Treatment Centres across Australia and New Zealand, the specialised haemophilia physiotherapists have been trained to use ultrasound imaging to more closely monitor joint health.
In addition to our normal physical assessment, known as the Haemophilia Joint Health Score, we will be performing an imaging protocol called the Haemophilia Early Arthropathy Detection with Ultrasound (or HEAD-US for short). This means we will be using the ultrasound scanner to look at the elbows, knees and ankles. These are the joints most commonly prone to bleeding episodes. In order to detect and grade any changes to the synovium (which is the layer surrounding the joint which helps produce fluid to keep the joint lubricated); the cartilage (the protective coating covering the bone ends); and the bones.
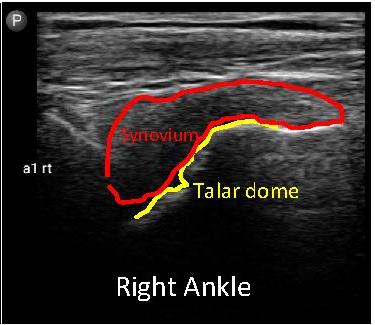
As we know, even one bleed into a joint can cause subtle changes to the joint as a whole, and more than one bleed can substantially alter the synovium, cartilage and eventually the bone surface itself. When a bleed occurs, the blood that leaked into the joint is removed by the synovium but the process of this irritates and inflames it, causing it to grow. This then makes it easier to pinch the synovium when the joint is moving, triggering another bleed. This leads to a vicious cycle of more frequent bleeds and more damage and changes occurring. Detecting these changes early and taking measures to stop this from happening will help to minimise this cycle and keep the joints as healthy as possible.
The HEAD-US protocol is being used in other countries as well as Australia and New Zealand with great success. A research study to look at the effectiveness of the HEAD-US protocol demonstrated that it was able to identify a greater proportion of joint abnormalities than physical assessment with the Haemophilia Joint Health score. However, this is not to say that the joint score is no longer useful as it is still able to identify other issues which cannot be detected by imaging alone.
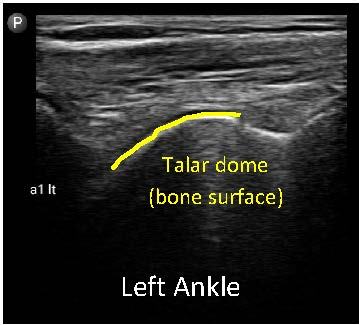
Within the Haemophilia Treatment Centre in Auckland, New Zealand this ultrasound protocol has been invaluable to assist in guiding treatment and identifying issues early. One such case involved a seven-year-old boy with severe haemophilia who had experienced three bleeds in the same ankle over a seven-month period. On physical examination there was only a small amount of swelling to the ankle and a very slight reduction in range of movement compared to the other side. However, when we used the ultrasound to look deeper inside the joint, we were able to identify significant changes to the synovium, cartilage damage and changes to the growth of the bones in his ankle (see images).
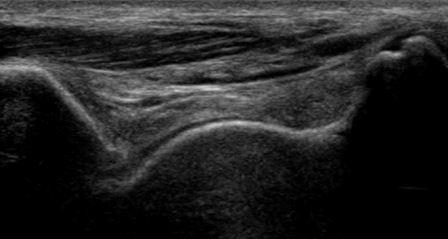
Image 1: Scanning plane

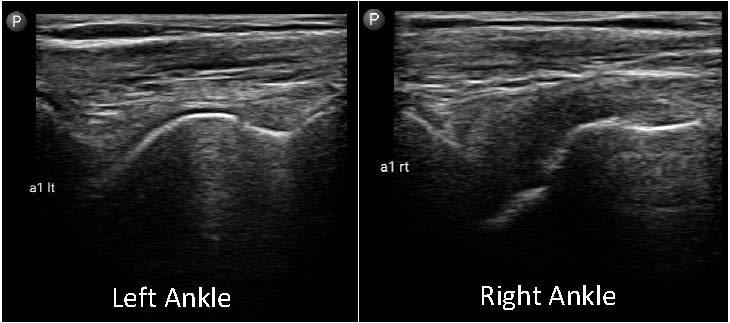
Image 2: normal anatomy seen in this plane
Images 3, 4 and 5: images of the ankles for case study patient 1
It was clear we needed to get better control over the bleeding episodes in his ankle. As a result, we increased his clotting factor prophylaxis dosage and provided more education to the patient and his family on how to recognise bleeding episodes. His blood was checked to monitor his response to the clotting factor replacement therapy and he was advised to reduce his activity levels for a while to allow the synovium time to settle and reduce the chance of further bleeding.
In another case, a 23-year-old male was also found to have issues with his ankles. In this instance he had not experienced any recognised bleeding episodes in his ankles for over seven years, although he had experienced frequent ankle bleeds as a child. On physical examination his ankles appeared to be slightly more swollen than observed at his last assessment (one year earlier) and there was a small reduction in his ankle movement compared to previous measures taken. Again using the ultrasound scanner and following the HEAD-US scanning protocol it was possible to identify changes to the synovium, cartilage and bone in keeping with a chronic synovitis (the synovium had become enlarged and he was experiencing repeated small bleeding episodes within the joint). In order to manage this more optimally we again made changes to his clotting factor dosing and regime. He was also educated on how to recognise and manage bleeding episodes and was advised on the benefits of weight loss for reducing joint loading. In addition, he was referred for a corticosteroid injection into the ankle. Corticosteroid is a strong anti-inflammatory agent which when injected into the joint can help to settle inflammation of the synovium, allowing it to shrink and reduce the risk of it getting caught in the joint and producing a bleed again.
These are just two examples of cases which have benefitted from the ultrasound, with many more untold stories and future successes to come. If you have any questions about the use of ultrasound, please speak to your local Haemophilia Treatment Centre.
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine