NICOLA HAMILTON
Nicola Hamilton is the haemophilia physiotherapist at the Royal Children’s Hospital, Melbourne
Plenary 3 – Pain
Chair ~ Dr Liane Khoo
Pain in haemophilia ~ Paul McLaughlin, UK
I enjoyed this presentation on pain and haemophilia as Paul McLaughlin, a leading haemophilia physiotherapist at the Royal Free Hospital in London, skilfully took us through an overview of pain and its complexities.
Paul explained that pain is complex and pain in haemophilia is even more complex. Pain can be acute from a joint or muscle bleed or it can be chronic from haemophilic arthropathy. For people with haemophilia, historically pain has been seen as a sign of bleeding and this has been taught from an early age.
Often pain is seen only through a biomedical lens and seeing pain ONLY as a correlation between joint health and joint status could be limiting.
Pain, however, can be distressing and it can interrupt your life and become a real problem.
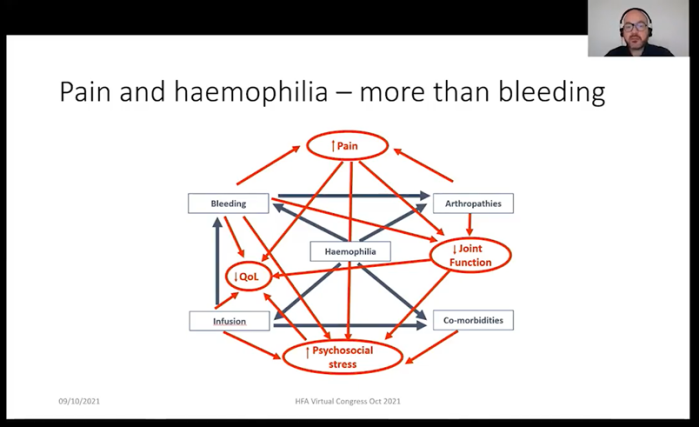
In haemophilia, pain is more than just bleeding. Pain can be both acute and chronic and both acute and chronic pain can happen at the same time. Pain can be distressing and interfere with daily mobility and being able to attend school and work.
Pain can increase with age and can increase with the number of joints affected by haemophilic arthropathy. It can increase when mental health and wellbeing is affected and it can increase when your quality of life is impacted or activities of daily living become more difficult.
Paul explained that pain is not linear. Yes, it can be caused by an injury or bleed, but it can also be influenced by personal, social, psychological, familial, and medical issues.
And what I though was incredibly important is that pain is always a personal experience, and everyone’s experience of pain is different.
Paul highlighted that when looking at pain, assessment is important and best addressed in a comprehensive care setting by a multidisciplinary team. Because pain in haemophilia can be complex, it is very important that we try and ascertain which pain we are assessing e.g., is it acute pain from a bleed or an arthritic pain or is it a pain from another cause. A thorough physical assessment is essential and as a physiotherapist, this for me is paramount. Working out what pain we are assessing can be difficult, so an assessment also means listening and talking to the person with haemophilia and trying to gain an understanding of their pain and how it is affecting them and their story.
Paul made some key points about managing pain and drew on not only the haemophilia world when it comes to pain management but the wider pain community. I think as clinicians we need to get better at looking beyond the haemophilia space, especially when it comes to chronic pain and its complexities.
Managing acute pain in haemophilia can be relatively straightforward. Acute bleeding episodes tend to happen at home and over time the person with haemophilia develops strategies that work for them. In a sense they become the expert in treating their bleeds and what works for them should not be discounted. It is important however that when the pain management strategies being used at home are not working, the person needs to contact their Haemophilia Treatment Centre (HTC) for further help and advice.
Managing chronic pain in haemophilia needs to be a partnership between the person with haemophilia and the comprehensive care team. It should be framed as health maintenance and person-centred, and consider the biological, psychological, and social influences that there may be on that person's chronic pain. It is about finding what matters to the person with haemophilia and working towards it, being goal orientated and potentially using a mix of approaches. People with chronic pain should be encouraged to move every day, even if it is just a little bit. Pain is not always as sign of damage or that things are getting worse – remember exercise is safe for most people with haemophilia.
The take home messages for me from this presentation were:
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine