SUE WEBZELL
Sue Webzell is the Haemophilia Clinical Nurse Specialist at Hollywood Private Hospital, Perth, WA
Plenary 1 – The changing world of bleeding disorders
Chair ~ Dr Ritam Prasad
Short personal stories
Overview of the Australian experience – spectrum of changes in bleeding disorders over the years ~ Prof Huyen Tran
Are we there yet? The innovative future of bleeding disorders treatment ~ Dr David Lillicrap, Canada
An overview of the impact of advances in treatment on quality of life and independence and on clinical practice ~ Dr Liane Khoo
Plenary 4 – Where to from here?
Chair ~ Dr Ritam Prasad
Haemophilia care in 2030 ~ Prof Michael Makris
Where to from here? ~ Dr David Stephensen
My vision for treatment and care into the future ~ Claudio, Alan, Shauna
Bleeding disorders treatment and care into the future ~ Dr Ritam Prasad
Where to from here? Achieving the vision ~ Sharon Caris
Panel discussion/Q&A
The focus on patient experiences around the changes in their treatments throughout the conference was a good reminder of the positive outcomes newer approaches to treatment have had on quality of life. The patients described improvement through less frequent treatments, easier administration routes or, very importantly, reduced bleeding episodes. The less their dependence on factor replacement, the more similarity they experienced to peers with better freedoms and travel opportunities. One patient’s experience showed significant improvement from anxiety and dependence using the original treatment to a feeling of freedom and independence on his current treatment.
The evolution of support services and treatment approaches from 1950s to now and into the future was a theme seen throughout many of the sessions. In the last two decades significant increases in scientific knowledge and understanding have led to changes in treatments, with various other treatment options under investigation at the current time.
Professor Huyen Tran outlined some of the advances in prophylaxis treatment. It is known there is an increased likelihood of bleeding the longer the factor levels are low. Home prophylaxis treatment with plasma-derived and recombinant clotting factors has been used within the last two decades to reduce the time at low factor levels and therefore reduce bleeding episodes. However, with standard half-life treatments, infusions were frequent and would sometimes result in poor adherence to the treatment regimen.
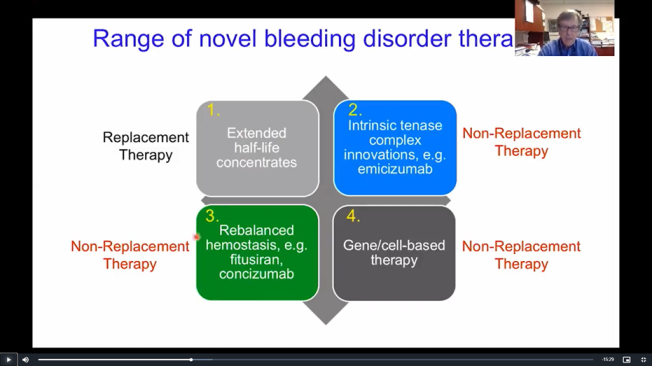
More recently extended half-life (EHL) therapies have been used in both haemophilia A and B, which remain active for longer periods and reduce the treatment burden for patients and their families by reducing the frequency of infusions. The reduced number of infusions has been seen to increase adherence to the treatment regimen and reduce bleeding episodes in general, with more patients seeing zero bleeds.
The biggest improvement is in haemophilia B where dosing for some individuals has decreased from 104 infusions a year (3-4 times weekly) to as few as 18-36 infusions a year (every 10-21 days).
In November 2020 emicizumab (Hemlibra®) became available in Australia for treatment of haemophilia A with or without inhibitors, the first of the new non-factor therapies to be publicly funded. This saw a huge change in treatment from the conventional intravenous factor replacement therapy to a subcutaneous injection of non-factor treatment. These non-factor therapies enable coagulation to occur without the need to replace the missing factor VIII. They allow for a steady state in factor levels without the peaks and troughs seen in conventional replacement factor therapy. Bleed rates in patients having emicizumab were significantly reduced, with reported improvements in quality of life, less bleeds, less sick days and reduced hospitalization.
Dr David Lillicrap spoke about the innovations in bleeding disorders treatments in recent years, the treatments in the pipeline and the science behind them. This was revisited by Prof Mike Makris in the final plenary, where he looked at the likely uptake of these treatments in the next decade.
Gene therapy is currently in clinical trial and for some individuals seems to allow for good factor levels for many years. However, it is not expected that it will be widely used, with around 10% of people with severe haemophilia are expected to receive it when it eventually becomes available. The funding process for this treatment would be complex and it is likely to be several years before this may become available. Currently gene therapy for factor IX deficiency seems to have better long-term factor expression.
Other novel non-factor treatments being investigated aim to rebalance coagulation by interfering with those naturally occurring products which would generally prevent thrombosis when present. By reducing the levels of these natural products, it is expected the bleeding risk could be reduced despite a lack of factor.
Prof Mike Makris speculated that in 2030 50% of patients will use non-factor products, 40% factor-based intravenous therapy and 10% gene therapy. Use of conventional factor products and adjunct therapies for individuals will still be required especially for surgery in non-severe patients.
Dr David Stephensen spoke about the impact of new treatments on quality of life and the role of physiotherapy into the future. Better management with treatments reducing bleeds should in turn reduce joint bleeds and arthropathy and the pain associated with these joint problems. Previously physiotherapy treatment was available for few and focused on limiting impairment by movement avoidance; now treatment for all individuals aims to maximize quality of life by maintaining physical and social wellbeing. Traumatic bleeds may still occur on these treatments, but spontaneous bleeds are significantly less likely on the newer treatments.
Sessions on virtual health and getting older contributed to the general discussion about where treatment for bleeding disorders is going in the future.
Telehealth and video consultations are here to stay but will be used alongside traditional face-to-face healthcare delivery systems. Seeing a person face-to-face can be more informative to determine a treatment plan but Scott Russell’s research study in the Virtual Health session showed that video consultations were a much better option for review than a standard telephone call, with more perceived confidence in the treatment plan when there was visual information alongside the verbal information.
Healthcare priorities should include best practice care and treatments for patients using comprehensive care strategies, with guidance from patient experience and goals for a personalized patient management and treatment plan. Patients with haemophilia are living longer with better treatments so the health conditions of ageing are now becoming a more common experience for the first time. Haemophilia Treatment Centres may need to adapt to better suit these changing patient requirements in the future.
Despite the great improvements in understanding and treatments for haemophilia, there have been limited changes being seen in von Willebrand disease (VWD) and other rare bleeding disorders. Research is being done around the disease biology which in time may lead to improvements in therapies.
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine