SUZANNE O'CALLAGHAN
Suzanne O'Callaghan is HFA Policy Research and Education Manager
Pain is a significant issue for many people with bleeding disorders. It can be pain related to a bleed or pain from complications, such as the haemophilic arthropathy or arthritis that results from repeated bleeding into a joint. Pain is not limited to older adults: people with bleeding disorders experience pain over their lifetime, from childhood through to old age.
The session on pain at the recent Australian Conference was a great opportunity for presenters to explore issues around pain from different perspectives.
This is a summary of the discussion, but if you are interested, some of the presentations are available online for you to watch in full. Visit the Conference presentations page to watch the videos.
20th Australian Conference on Haemophilia, VWD and Rare Bleeding Disorders

Chair ~ Dr Liane Khoo
What’s new in pain? Is it different now with new treatments? ~ Dr Liane Khoo
Pain in haemophilia ~ Paul McLaughlin, UK
A body and mind approach for pain management in people with bleeding disorders ~ A/Prof Carolyn Arnold
Patient personal perspective on chronic pain ~ Jane Portnoy, haemophilia social worker interviewing Dylan
Osteoarthritis, exercise and pain: the GLA:D® program ~ Dr Christian Barton
Dr Liane Khoo, Haemophilia Treatment Centre Director at the Royal Prince Alfred Hospital, Sydney, introduced the session by commenting that pain management is an important part of treatment and care for haemophilia.
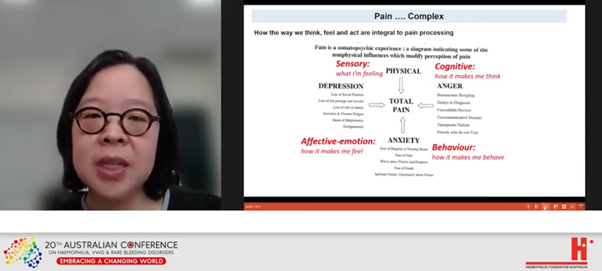
‘It is a biopsychosocial experience. It is beyond the mere concept of nociception, or the brain processing pain,’ she said.
While the physical pathology at the site of an injury such as a joint bleed needs to be identified, this is not enough to explain ‘the complex process by which pain is transformed into the physiological, cognitive, affective and behavioural responses labelled as pain. How we think, feel and act are integral to pain processing.’
Paul McLaughlin followed with a fascinating discussion of pain and its complexities from the point of view of a haemophilia physiotherapist. You can read more on his presentation in Pain and haemophilia in the December 2021 issue of National Haemophilia.
A/Prof Carolyn Arnold specialises in pain management at The Alfred hospital in Melbourne and walked through some of the recent changes to pain management.
She highlighted that a holistic approach to pain management is essential.
New and innovative haemophilia treatments have made a substantial difference to the experience of acute pain, reducing the number and severity of bleeding episodes. This will also impact on joint degeneration from bleeding into joints.
Knowing the cause of pain is important – if it is a bleed, synovitis, haemophilic arthropathy or sensitisation. However, what can be seen on an X-Ray or other imaging is only one part of understanding pain.
As people with haemophilia grow older, the experience of pain can be disproportionate to what can be seen clinically, with the pathology of a joint, for example. This can be due to ‘sensitisation’ within the sensory system and it is important to manage pain and have pain free intervals to minimise this sensitisation.
With repeated episodes of injury with pain, the person’s ability to recover reduces and chronic pain can result, along with an inability to tolerate as much activity – known as the ‘boom and bust cycle’. ‘The art is to find the right amount of activity to function better on every day and maintain your strength and mobility.’
How to do this?

While medications may be used, they need to be used wisely and other non-drug options will be very important, as part of a ‘healthy, happy, resilient lifestyle approach'. This consists of:
She spoke about avoiding the hazards of chronic pain – its impact on reduced fitness, strength and balance, on mental health, relationships, work, social isolation and over-reliance on drugs.
She also drew attention to the information about pain on the website www.painrevolution.org, which is a program for regional and rural Australia, but has valuable information for everyone.

When our understanding of pain is so subjective, hearing the patient experience is crucial. Jane Portnoy, Haemophilia Social Worker at The Alfred in Melbourne, interviewed Dylan, a young man with haemophilia A, about pain and how it has affected him. Dylan’s articulate comments on his experiences gave great insight into the day-to-day impact of pain.
Dylan explained that it is often difficult to explain his pain to the Haemophilia Team – what he is feeling, how long he has had the pain, how he would describe the pain. ‘It can be a really frustrating experience when people don’t seem to understand what you are going through as a haemophilia patient,’ he said.
Another significant aspect was the impact of pain on limiting his life: his career, his social life, his mental health, exercising. ‘It’s hard not to put some blame onto yourself because you are constantly worrying that the things that you are doing everyday are causing your pain,’ Dylan remarked.
How does he manage his pain?
His biggest barrier?
His suggestion to others?
Surprisingly, the recommended first line treatment for osteoarthritis in the knee and hip is exercise, education and weight control, no matter what the severity of pain.
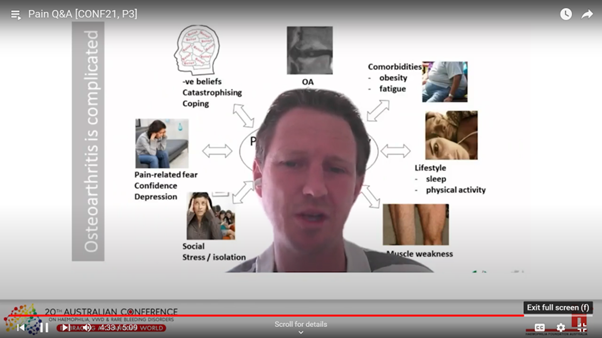
Dr Christian Barton walked through the research and the international GLA:D® program that is led in Australia by his team at LaTrobe University, Melbourne. His key messages:
The GLA:D® (Good Life with osteoArthritis: Denmark) program is an education and exercise program developed by Danish researchers for people with hip or knee osteoarthritis symptoms. It is now available across Australia, delivered by physiotherapists who are trained and led by the LaTrobe team. The focus of this program is to change the way people think about their joints and pain, and the many factors that can affect and improve their pain and mobility, using exercise and education as strategies. Dr Barton explained there are a range of exercises aimed at building confidence – you can find examples online at the free open-source website https://nemex.trekeducation.org/.
An important take-home message from his session was that exercise therapy needs to address the commonly held myth that exercise is detrimental to arthritis and deal with the barriers to participating in exercise.
The session finished with questions from the audience.
What can you recommend for family and carers who feel so helpless when our loved ones are in pain?
A/Prof Carolyn Arnold answered:
This was a rewarding and enlightening session about an issue of concern to most people with bleeding disorders and the full presentations are well worth watching.
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine