AISHA BARTON-ROSS
Aisha Barton-Ross is a physiotherapist with the haemophilia team at the Royal Children’s Hospital, Melbourne
The COVID-19 pandemic has brought virtual care – both challenges and benefits – to the forefront of healthcare, which was a key theme in a number of sessions I attended at the 2022 WFH World Congress in Montreal. Poignantly, the Congress was held as a hybrid online and face-to-face event this year in light of ongoing travel restrictions brought on by the pandemic. Two sessions covered some highly relevant issues in expanding virtual haemophilia care.
Hot topic debates – Tele rehabilitation: yes or no?
Chair ~ Adolfo Llinas, Colombia
Speakers:
Yes ~ Peter Aguero, Physiotherapist, University of California, San Diego, USA
No ~ Mark Krimmel, Physical Therapist, Washington Center for Bleeding Disorders, Seattle, USA

The pros and cons of tele-rehabilitation were debated in the Hot Topics session. The speakers emphasised that virtual care is not a ‘one size fits all’ model but demonstrates clear benefits for some patients. They discussed a number of benefits and limitations of tele-rehabilitation:
| Benefits | Limitations |
|
|
Peter Aguero took the ‘pro’ position and highlighted how telerehabilitation fits into the realm of evidence-based practice.

Source: What is evidence-based practice? Simmons University Library Guide, 2012 – simmons.libguides.com/ebsw
I thought this was a great way of highlighting that providing the best evidence-based care does not simply rely on what best research is available. At present, the body of research evidence behind face-to-face assessment and treatment is greater. However, given that virtual care provision is still emerging, that does not discount the merit of virtual care, especially when the patient’s needs, available resources and the environmental context are considered. The discussion following this session also highlighted that although virtual care should be considered another ‘tool in the toolbox’, it needs to be individualised to the to the patient and their situation.
Use of technology with patients
Chair ~ Marlène Beijlevelt, Hemophilia and Research Nurse, Amsterdam UMC, Netherlands
Telemedicine ~ Helen Manson, Haemophilia Sister, Belfast Health and Social Care Trust, UK
Helen Manson outlined how a virtual model of care had been integrated into the haemophilia space and talked about the steps involved in launching a novel virtual multidisciplinary team (MDT) haemophilia clinic from the Northern Ireland Haemophilia Centre in Belfast in 2020.

In January 2020, nursing and physiotherapy teams started work with the hospital IT department to explore a proof-of-concept study prior to launching a pilot virtual MDT clinic. This included developing resources for both clinicians (Microsoft Teams training, a video consultation etiquette guide, and a clinic script to standardise key assessment measures) and patients (information leaflet and telehealth guide) to ensure both parties were prepared for the virtual clinic format. Electronic patient and clinician feedback forms were also developed across the project. The pilot clinic was launched in May 2020, in somewhat opportune timing, shortly after COVID-19 restrictions were put in place. Once feedback from the pilot clinic had been analysed, the full virtual MDT clinic was launched.
Five virtual MDT clinics with a haematologist, nurse, physiotherapist, and social worker were then held between May and July 2020, with 28 patients participating. Interestingly, compared with an audit of face-to-face clinics across a comparable time period, attendance rates were more than 20% higher in the virtual clinic and the mean time per consultation was more than halved. Though feedback from patients was extremely positive, benefits and limitations mimicked those discussed in the previous sessions.
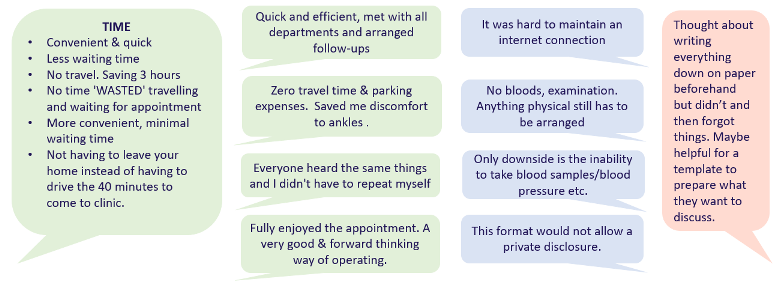
Feedback about the virtual clinic
Slide published with permission from Helen Manson, Belfast Health and Social Care Trust
I thought this model highlighted two key elements both physiotherapy and wider multidisciplinary health services should be target when considering a virtual care model: ensuring adequate training and preparation for both clinicians and patients, and ensuring feedback is regularly encouraged so that the service can continue to be refined.
The take-away messages from these sessions for me were:
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine