What is haemophilia?
Haemophilia is a bleeding disorder where blood doesn’t clot properly. It occurs when blood does not have enough clotting factor. A clotting factor is a protein in blood that controls bleeding.
There are two types of haemophilia. Both have the same symptoms.
- Haemophilia A is the most common form and is caused by having low levels of clotting factor VIII (8). It is also called factor VIII deficiency.
- Haemophilia B is caused by having low levels of clotting factor IX (9). It is also called factor IX deficiency.
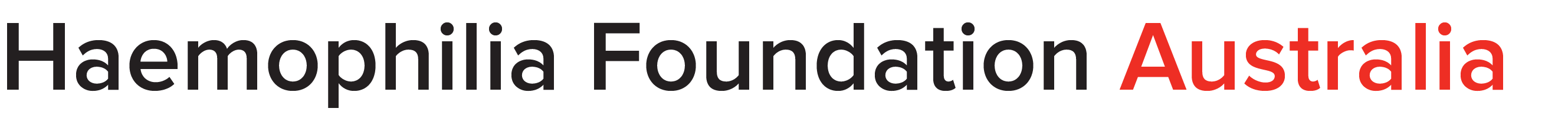
There are different levels of severity in haemophilia: mild, moderate and severe. This is linked to the amount of clotting factor in the blood.
Haemophilia is not contagious. It is a genetic condition and a person with haemophilia is born with it. It can be inherited and passed on from parent to child.
What causes haemophilia?
Everyone has the gene that makes clotting factor VIII (the factor 8 or F8 gene) and the gene that makes clotting factor IX (the factor 9 or F9 gene). These factors are needed for blood to clot.
Haemophilia is caused by a change (mutation or alteration) in the F8 or F9 gene. The gene does not work as well as it should. As a result, the body does not make enough factor VIII (8) or factor IX (9) for blood to clot properly.
How common is haemophilia?
Haemophilia is rare. It occurs in all races and socio-economic groups.
Haemophilia in males
Men and boys with the F8 or F9 gene alteration always have haemophilia.
- Approximately 1 in 6,000 males has haemophilia A
- Approximately 1 in 25,000-30,000 males has haemophilia B (2,5)
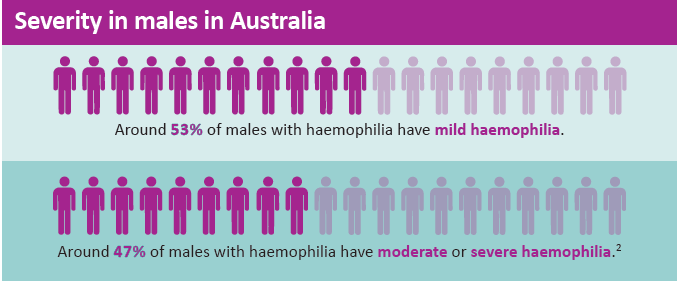
Haemophilia in females
Researchers are currently investigating worldwide to understand how haemophilia affects females and how common it is. (1,3,4)
What happens when you have haemophilia?
If you have haemophilia, you will have what is called a bleeding tendency. This means you are likely to bleed more often than other people.
A person with haemophilia does not bleed any faster than anyone else, but bleeding can continue for longer if it is not treated. This results in poor healing. Minor bruising or scratches on the skin are not usually a problem.
For people with haemophilia, situations become more serious when there is internal or prolonged bleeding. If normal first aid does not stop the bleeding, without other treatment the bleeding can continue for days. Specialised treatment will be needed so blood can clot normally.
Women and girls may have heavy and/or long menstrual periods. This is called heavy menstrual bleeding or sometimes abnormal uterine bleeding or menorrhagia. It can lead to anaemia (low levels of red blood cells or iron in the body).
Some women may also have heavy bleeding for a long time after childbirth.
Bleeding can occur internally in any part of the body, including muscles and joints, particularly after an injury or surgery. Bleeding can also occur into organs such as the brain. People with haemophilia should always seek medical advice after a blow to the head to make sure it has not caused internal bleeding.
It is important for people with haemophilia to involve their haemophilia treating team with any medical or dental procedures or surgery – anything larger than a blood test – to make sure it is managed safely.
Treatment
Haemophilia is a lifelong condition. It can’t be cured yet, but with current treatments it can be managed effectively.
Haemophilia treatment helps the blood to clot and promotes healing.
Treatment may be used to prevent bleeding episodes or control a bleeding episode once it starts.
For more information on treatment, see the YOUR DIAGNOSIS AND TREATMENT section