SUZANNE O'CALLAGHAN
Suzanne O'Callaghan is HFA Policy Research and Education Manager
Von Willebrand disease
Chair ~ Susie Couper
VWD personal experience ~ Perry
VWD genetics, diagnosis and classification ~ Dr Simon McRae
VWD personal experience ~ Simoni
VWD treatment and future directions ~ Dr Nathan Connell
The von Willebrand disease session brought together some of the key players in the development of the new international clinical VWD guidelines to discuss the implications for diagnosis, treatment and care into the future.
Setting the scene from the perspective of the patient were two compelling personal experiences from Perry and Simoni.
As an older man with type 2A VWD, Perry had not been diagnosed until he was in his 50s. He spoke about the problems he experienced with bleeding episodes over his lifetime before he was diagnosed and had a treatment plan – nose and mouth bleeds, lengthy bleeding after surgery. This bleeding is now much better controlled in liaison with his Haemophilia Treatment Centre.
Simoni is a young woman with type 3 VWD and was diagnosed as a young child after bruising severely. As she has grown up, she has had a number of bleeding problems, including heavy menstrual bleeding and bleeds after sports injuries. For Simoni, starting prophylaxis was a turning point for taking control of her bleeding and her quality of life.
You can read Perry and Simoni’s personal stories in this issue of National Haemophilia.
What is exciting about the new international guidelines from a patient perspective? As a patient representative in the international panel for the clinical management guidelines, Susie Couper had three reasons to be excited:
Dr Simon McRae, now based at Launceston General Hospital in Tasmania, was a member of the international panel for the VWD diagnostic guidelines. He explained that there had been some variations in diagnostic criteria in previous guidelines and the new guidelines had been an opportunity to develop some consistency and provide decision-making tools.
The guidelines considered:
The circumstances of diagnosis were very relevant.
A BAT would be useful if a patient was being seen at a primary care setting, eg a GP clinic, where the likelihood of them having a bleeding disorder was lower. A validated BAT could identify those who have abnormal bleeding that falls into the type of bleeding seen in a bleeding disorder such as VWD and indicate where further testing is appropriate.
If a patient has been referred to a haematologist or has a strong family history, they are more likely to have a bleeding disorder and a BAT is not needed to decide about testing. However, a BAT can be useful to help define their particular bleeding pattern.
Other areas that the guidelines clarified were:
The guidelines also considered questions such as differentiating between type 1 and type 2 and when VWD genetic testing is useful (ie, for type 2A, 2B or 2N and for family planning in type 3).
What are the implications of the new diagnostic guidelines for Australia?
Dr McRae pointed out that the guidelines won’t change diagnostic practice in most Australian settings and are unlikely to change patient management for individuals. They are likely to lead to a review of current diagnoses in the ABDR and there may be a need to retest patients where insufficient information is available. This will take some time. However, an important outcome for patients will be standardising of the wording for individual diagnoses, including on the ABDR patient card.
He also recommended a national network approach for genetic testing and some functional assays. Genetic testing funding is not always available nationally, making it difficult in some cases to work out how to fund the tests that are required for accurate and timely diagnosis.
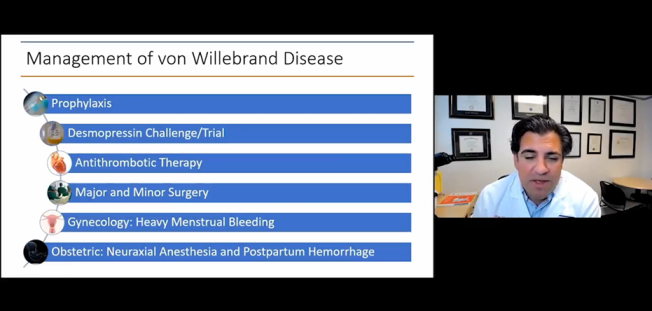
Dr Nathan Connell gave an update on the latest developments in VWD treatment, based on the new international VWD guidelines. Dr Connell was Vice-Chair of the international VWD guidelines Scoping Group and explained that the Group was an international partnership to develop evidence-based clinical management guidelines to promote better health outcomes, quality of life and health equity.
He discussed some of the key questions covered by the guidelines.
Prophylaxis is recommended for type 3 (severe) VWD, but conditionally – a shared decision-making process between the doctor and the patient.
The recommendations for heavy menstrual bleeding:
For people with mild and moderate VWD, what are the ‘moments that matter’, the triggers to get in contact with their Haemophilia Treatment Centre (HTC)?
Both Simon McRae and Nathan Connell pointed to a real need for evidence-based research to answer a range of questions about VWD, for example:
We were grateful to all the presenters for sharing their expertise and their personal stories. The expert presentations from Simon McRae and Nathan Connell were immensely valuable and gave a concise and accessible overview of priority issues in VWD diagnosis and treatment. Having the personal perspectives of Susie, Perry and Simoni alongside their presentations grounded the discussion about the guidelines in real-life experience – and highlighted just why the process of developing international guidelines has been so important.
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine